VARICOSE VEINS
Definition
Varicose veins are dilated, tortuous, elongated superficial veins that
are usually seen in the legs.
Description
Varicose veins, also called varicosities, are mostly often on the legs,
although they can be found in other parts of the body. Mostly they
appear as lumpy, winding vessels just below the surface of the skin.
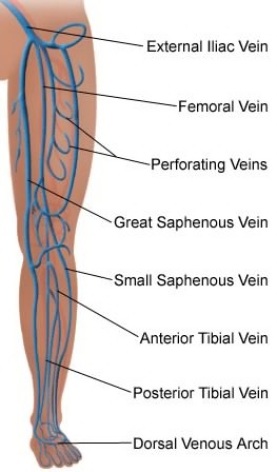
There are three types of veins –
- Superficial veins that are just beneath the surface of the skin.
- Deep veins that are large blood vessels found deep inside muscles.
- Perforator veins that connect the superficial veins to the deep veins.
The superficial veins are the blood vessels most often affected by varicose veins and are the veins seen by eye when the varicose condition have developed. The inside of veins have valves that open and close in response to blood flow. When the left ventricle of the heart pushes blood into the aorta, it produces high pressure pulse of heartbeat and pushes blood throughout the body.
Between heartbeats, there are periods of low pressure. During these low pressure periods, blood in the veins are affected by gravity and turns to flow downward. The valves in the veins prevent this from happening. Varicose veins
start when one or more valves fail to close. The blood pressure in that section of vein increases, causing additional valves to fail. This allows a pool of blood in that location and stretches the veins, further weakening the walls of the veins. The walls of the affected veins lose their
elasticity in response to increased blood pressure. As the vessels weaken,more and more valves are unable to close properly.
The veins become larger and wider over time and begin to appear as lumpy, winding chains underneath the skin. Varicose veins can develop in the deep veins also. Varicose veins in the superficial veins are called primary varicosities, while varicose veins in the deep veins are called
secondary varicosities.
The other type of veins to observe during thrombophlebitis and normal appearance of leg muscles veins is Varicose (Spider) veins.

What are bulging veins?
Bulging of the veins is a symptom that commonly occurs in different conditions, such as thrombophlebitis, pregnancy, older age, and congenitally defective valves in the veins. Varicose veins are dilated, often distorted, and swollen veins that may be painful. Varicose veins are most frequently seen in the legs.
Veins have valves that act as one-way flaps to prevent blood from flowing backward as it moves up the legs. Bulging of the veins results when the valves do not function properly, allowing the blood to pool and enlarge the vein. It may occur in conditions affecting the vein itself or in association with more generalized conditions, such as pregnancy and aging. Inflammation and swelling of a vein (thrombophlebitis) is a common cause of bulging veins. Other common causes include lack of movement and obesity. Obstructions to the flow of blood in the veins can also cause bulging.
Pregnancy can lead to bulging veins in some women. Pregnancy increases the volume of blood within the body but decreases the flow of blood from the legs to the pelvis. The decreased blood flow from the legs can result in bulging veins in the legs. Bulging veins may worsen during late pregnancy, when the uterus exerts greater pressure on the veins in the legs.
Advancing age can also cause bulging veins. The aging process can cause veins to weaken and lose elasticity, and they become unable to effectively push the blood back toward the heart. As blood pools in the veins, they become enlarged and bulge.
In some cases, bulging of the veins can be a symptom of a serious condition. Seek prompt medical care if you experience bulging veins along with skin ulcers or sudden swelling in the area of the bulging veins. These are symptoms of peripheral vascular disease and blood clots. In addition, if bulging veins are persistent or calls for concern, seek prompt medical care.
What other symptoms might occur with bulging veins?
Bulging veins may accompany other symptoms, which vary depending on the underlying disease, disorder or condition. Symptoms that frequently affect the veins may also involve other body systems.
Leg symptoms that may occur along with bulging veins
Bulging veins may accompany other symptoms affecting the legs including:
- Aching pain that may get worse after sitting or standing for a long time
- Darkening of the skin
- Feeling of heaviness in legs
- Rash that is itchy or irritated
- Swelling
- Throbbing or cramping
Other symptoms that may occur along with bulging veins
Bulging veins may accompany symptoms related to other body systems including:
- Symptoms of diabetes, such as damage to blood vessels, skin ulcers near the ankle, and slow-healing wounds
- Symptoms of obesity, such as increased weight and inactivity
- Symptoms of pregnancy, such as increased weight, increased blood volume, and pressure in abdomen
- Symptoms of thrombophlebitis, such as inflammation, pain, and redness or warmth of the skin in the affected area.
Symptoms that might indicate a serious condition
In some cases, bulging veins may occur with other symptoms that might indicate a serious condition that should be immediately evaluated in an emergency setting. Seek immediate medical care (call 911) if you, or someone you are with, have bulging veins along with other serious symptoms including:
- Bleeding from injury to the vein
- Feeling of pulling or pain in the leg
- Redness, warmth or swelling in the leg
- Skin on the ankle or calf thickening and changing color
- Sores or skin ulcers on the leg or ankle.
What causes bulging veins?
Bulging veins usually result from weak or damaged valves in the veins. The heart pumps blood that supplies oxygen and nutrients to the whole body through the arteries. Veins then carry the blood from the body back to the heart. As leg muscles contract, they push blood back to the heart from the lower body against the flow of gravity. Veins have valves that act as one-way flaps to prevent blood from flowing backward as it moves up the legs. If the valves become weak, blood can leak back into the veins and collect there, making the veins bigger and bulging.
Causes of bulging veins
Bulging veins can be caused by different conditions. Although rare, tumors and infections may exert pressure on the veins in a localized area, resulting in bulging and congestion of the veins. Causes of bulging veins include:
- Abdominal tumor or mass
- Aging
- Blood clot
- Inactivity
- Extraneous activities such as weight lifting
- Pregnancy
- Structural abnormality of valves in the veins
- Swelling
- Exhaustion exercises
- Thrombophlebitis
Serious or life-threatening causes of bulging veins
In some cases, bulging veins may be a symptom of a serious or life-threatening condition that should be immediately evaluated in an emergency setting. These include:
- Blood clot
- Infection
- Tumor
Questions for diagnosing the cause of bulging veins
To diagnose your condition, your doctor or licensed health care practitioner will ask you several questions related to your bulging veins including:
- How long have you had bulging veins?
- Did you experience an injury to the area where you have bulging veins?
- Do you have any other symptoms?
- What medications are you taking?
What are the potential complications of bulging veins?
Because bulging veins can be caused by serious diseases, failure to seek treatment can result in complications and permanent damage. Once the underlying cause is diagnosed, it is important for you to follow the treatment plan you and your health care professional design specifically for you to reduce the risk of potential complications including:
- Blood clots
- Skin ulcerations near bulging veins
- Swelling and pain
Varicose Veins
| DRG Category: | 263 |
| Mean LOS: | 6 days |
| Description: | SURGICAL: Vein Ligation and Stripping |
| DRG Category: | 299 |
| Mean LOS: | 5.8 days |
| Description: | MEDICAL: Peripheral Vascular Disorders With Major CC |
What is DRG?
DRG Codes (Diagnosis Related Group) Diagnosis-related group (DRG) is a system to classify hospital cases into one of approximately 500 groups, also referred to as DRGs, expected to have similar hospital resource use. They have been used in the United States since 1983.
What is MDC?
The Major Diagnostic Categories (MDC) are formed by dividing all possible principal diagnoses (from ICD-9) into 25 mutually exclusive diagnosis areas. The diagnoses in each MDC correspond to a single organ system or etiology and in general are associated with a particular medical specialty.
CC Analysis Data Files: The CC analysis data file contains claims data that is use in the process
of classifying ICD-9-CM codes as a Major Complication or Comorbidity (MCC), CC or non-CC.
- MDC Code:Major Diagnostic Category
- MDC Description: Major Diagnostic Category Description
- DRG Code: Diagnostic Related Group
- DRG Description: Diagnostic Related Group Description
- Medical/Surgical: Major Diagnostic Category Medical or Surgical section
- GMLOS: Geometric Mean Length of Stay
- AMLOS: Arithmetic Mean Length of Stay
- RW: Relative Weight
- LOS: Length of Stay
- CC: Complication or Comorbidity
Varicose veins (varicosities) are the visible manifestations of abnormally dilated, tortuous veins. They occur most often in the lower extremities but can appear anywhere in the body. Primary varicosities
are caused by incompetent valves in the superficial saphenous veins, whereas secondary varicosities are the result of impaired blood flow in the deep veins.
Primary varicosities tend to occur in both legs, whereas secondary varicosities usually occur in only one leg.
In a ladderlike fashion, perforator veins connect the deep vein and the superficial vein systems, promoting drainage of the lower extremities.Blood can be shunted from one system to the other in the event of either system’s being
compressed. Incompetence in one system can lead to varicosities. Varicose veins are considered a chronic disease and
along with valvular (heart disease) incompetence, can progress to chronic venous insufficiency (CVI).
Causes
Primary varicose veins occur because of incompetent venous valves that result in venous hypertension. They occur most commonly at the saphenofemoral junction (SFJ). Several factors cause increased venous pressure and venous stasis that result in dilation and stretching of the vessel wall. Increased venous pressure results from being erect, which shifts the full weight of the venous column of blood to the legs. Prolonged standing increases venous pressure because leg muscle use is less; therefore, blood return to the heart is decreased. Secondary varicose veins result from deep venous thrombosis and its sequelae or congenital anatomical abnormalities.
Heavy lifting, genetic factors, obesity, thrombophlebitis, pregnancy,
trauma, abdominal tumors, congenital or acquired arteriovenous fistulae, and congenital venous malformations are among the causes of varicose
veins.
Chronic liver diseases such as cirrhosis can cause varicosities in the rectum, abdomen, and esophagus.
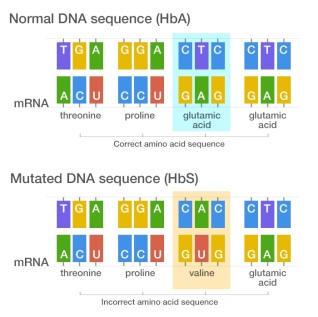
Genetic considerations
Genetic transmission of varicose veins has been reported since the 1950s with various modes of transmission suggested. Several loci have been identified through linkage analysis (FOXC2, LIPH), and candidate
genes are being further investigated. Disruption of production of the gene coding for vascular endothelial growth factor (VEGF) is one
implicated mechanism. Family history accounts for an estimated 20% of the risk of disease.
The FOXC2 gene provides instructions for making a protein that plays a critical role in the formation of many organs and tissues before birth. This protein is a transcription factor, which means that it attaches (binds) to specific regions of DNA and helps control the activity of many other genes. Researchers believe that the FOXC2 protein has a role in a variety of developmental processes, such as the formation of veins and the development of the lungs, eyes, kidneys and urinary tract, cardiovascular system, and the transport system for immune cells (lymphatic vessels).
What is DNA?
DNA, or deoxyribonucleic acid, is the hereditary material in humans and almost all other organisms. Nearly every cell in a person’s body has the same DNA. Most DNA is located in the cell nucleus (where it is called nuclear DNA), but a small amount of DNA can also be found in the mitochondria (where it is called mitochondrial DNA or mtDNA).

The information in DNA is stored as a code made up of four chemical bases: adenine (A), guanine (G), cytosine (C), and thymine (T). Human DNA consists of about 3 billion bases, and more than 99 percent of those bases are the same in all people. The order, or sequence, of these bases determines the information available for building and maintaining an organism, similar to the way in which letters of the alphabet appear in a certain order to form words and sentences.
DNA bases pair up with each other, A with T and C with G, to form units called base pairs. Each base is also attached to a sugar molecule and a phosphate molecule. Together, a base, sugar, and phosphate are called a nucleotide. Nucleotides are arranged in two long strands that form a spiral called a double helix. The structure of the double helix is somewhat like a ladder, with the base pairs forming the ladder’s rungs and the sugar and phosphate molecules forming the vertical sidepieces of the ladder.
An important property of DNA is that it can replicate, or make copies of itself. Each strand of DNA in the double helix can serve as a pattern for duplicating the sequence of bases. This is critical when cells divide because each new cell needs to have an exact copy of the DNA present in the old cell.
DNA is a double helix formed by base pairs attached to a sugar-phosphate backbone.
What is a gene?
A gene is the basic physical and functional unit of heredity. Genes, which are made up of DNA, act as instructions to make molecules called proteins. In humans, genes vary in size from a few hundred DNA bases to more than 2 million bases. The Human Genome Project has estimated that humans have between 20,000 and 25,000 genes.
Every person has two copies of each gene, one inherited from each parent. Most genes are the same in all people, but a small number of genes (less than 1 percent of the total) are slightly different between people. Alleles are forms of the same gene with small differences in their sequence of DNA bases. These small differences contribute to each person’s unique physical features.

Genes are made up of DNA. Each chromosome contains many genes.
A locus (plural loci) in genetics is the position on a chromosome. Each chromosome carries many genes; humans’ estimated ‘haploid’ protein coding genes are 19,000-20,000, on the 23 different chromosomes. A variant of the similar DNA sequence located at a givenlocus is called an allele.
What is a Locus?
A locus (plural loci) in genetics is the position on a chromosome. Each chromosome carries many genes; humans’ estimated ‘haploid’ protein coding genes are 19,000-20,000, on the 23 different chromosomes. A variant of the similar DNA sequence located at a given locus is called an allele.
Gender, ethnic/racial, and life span considerations
About 15% to 20% of all adults in the United States have varicose veins. Prevalence increases with age, peaking in the 50s and 60s and decreasing dramatically after age 70. Varicose veins are more common in women at the ages of 30 through 40, and we have seen dramatic difference as much as four times compare to their male counterpart. There are no known ethnic or racial dependency/considerations.
Global health considerations
Varicose veins affect an estimated one in five persons in the world.
The prevalence of venous disease and varicose veins is higher in developed than in developing nations, likely due to alterations in lifestyle, nutrition, body mass index and physical activity.
Assessment
History
Elicit a history of symptoms, paying particular attention to pain and discomfort, changes in appearance of vessels and skin, and complaints of a sensation of fullness of the lower extremities.
Ask the patient to describe the amount of time each day spent standing. Take an occupational history with particular attention to those jobs that require long hours of walking or standing.
Question the patient about lifetime weight changes, such as changes during pregnancy and sustained periods of being overweight. Ask the patient if there is a personal or family history of heart disease, obesity, or varicose veins.
Physical examination
Superficial veins can be inspected for distension and prominence as well as accompanying symptoms such as ulceration, swelling, blanching, and a sense of fullness of the legs. The number, severity, and type of varicosities determine the symptoms experienced by the individual. With
the patient standing, examine the legs from the groin to the foot in good lighting. Inspect the ankles, measure the calves for differences, and assess for edema. Time of examination is a factor
because secondary varicosities are more symptomatic earlier in the day. Palpate both legs for dilated, bulbous, or corkscrew vessels.
Patients may complain of heaviness, aching, edema, muscle cramps, increased fatigue of lower leg muscles, and itching. Severity of discomfort may be difficult to assess and is unrelated to the size of the varicosity.
Psychosocial
Some patients with varicose veins may occasionally experience progressively worsening condition depending on their activities. Assess patient for any problems with body image because of the changed appearance of skin surface that is caused by
varicose veins. Question patient to determine possible lifestyle adjustments to decrease symptoms. In addition to medical consultation, the patient may need change in nutrition, skin therapy, job counseling and/or occupational retraining.
Diagnostic highlights
General Comments: Incompetency of the deep and superficial veins can be
diagnosed by several tests.
| Test | Normal Result | Abnormality With Condition | Explanation |
| Duplex ultrasound (most commonly used diagnostic tool) | Normal Doppler venous signal with spontaneous respiration; no evidence of occlusion | Reversal of blood flow is noted as a result of incompetent valves in varicose veins | Detects moving red blood cells, thus demonstrating venous patency |
| Trendelenburg’s test | Veins fill from below in about 30 sec after the tourniquet is in place and the client stands; no further blood fills the veins from above after the tourniquet is released | Additional blood flows into the vein from above, indicating a valve is incompetent and has allowed a backflow of blood | Detects abnormal filling time and incompetent valves; veins normally fill from below; if the vein fills from above,
The incompetent valve is allowing blood to flow backward |
| Venous plethysmography(cuff pressure test) | Patent venous system without evidence of thrombosis or occlusion | Venous obstruction | Measures the volume of an extremity; rulesout a deep vein thrombosis |
| Magnetic resonance venography and magnetic resonance imaging | Normal blood flow without evidence of occlusion | Reversal of blood flow noted | Examines blood flow in extremities |
| Venography | No evidence of obstruction | Abnormal venous flow seen | Xray study designed to locate thrombosis in lower extremities |
Other Tests: Contrast venography and color-flow duplex ultrasonography
Primary nursing diagnosis
Diagnosis
Altered tissue perfusion (peripheral) related to increased venous
pressure and obstruction.
Outcomes
Tissue perfusion: Peripheral
Interventions
Circulatory care; Positioning; Pain management
Planning and implementation
Collaborative
MEDICAL
Treatment for varicose veins is aimed at improving blood flow, reducing injury,
and reducing venous pressure. Pharmacological treatment is not indicated for Varicose veins. To give support and promote venous return, physicians recommend wearing elastic stockings. If the varicosities are moderately severe, the physician may recommend antiembolism stockings or elastic bandages or,
in severe cases, custom-fitted heavy-weight stockings with graduated pressure. When obesity is a factor,
the patient is placed on a weight-loss regimen.Experts also recommend that the patient stop smoking
to prevent vasoconstriction of the vessels.
A nonsurgical treatment is the use of sclerotherapy for varicose
and spider veins. Sclerotherapy is palliative, not curative, and is often done for cosmetic reasons after surgical intervention.
A sclerosing agent,
such as sodium tetradecyl sulfate (Sotradecol), hypertonic saline, aethoxysclerol, or hyperosmolar salt-sugar solution, is injected into the vein, followed by a compression
bandage for a period of time.
SURGICAL
A surgical approach to varicose veins is vein ligation (tying off) or
stripping (removal) of the incompetent veins. Removal of the vein is performed through multiple short incisions from the ankle to the groin. A compression dressing is
applied after surgery and is maintained for 3 to 5 days. Patients are
encouraged to walk immediately post operatively. Elevate the foot of the bed 6 to 9 inches to keep the leg above the heart when the postoperative client is in bed.
Pharmacologic highlights
No medications are generally used to treat varicose veins, except for
analgesics following surgery.
Independent
Nursing interventions are aimed by educating the patient to decrease
venous stasis, promote venous return and prevent tissue injury.
To prevent vein distention by compression of superficial veins –
- In case of edema, teach patients to apply elastic support stockings before standing and to avoid long periods of standing if not necessary.
- Patients should be encouraged to engage in exercise programs,
walking, aquatic exercise programs in order to strengthen their legs muscles. - Teach patients to avoid crossing their when sitting for long periods of time and to elevate the legs when sitting or lying down.
- Patients should be taught to observe the skin when removing stockings to check for signs of irritation,
edema, decreased nerve sensation, and discoloration.
Preventive measures are similar to those patients with thrombophlebitis
For patients who have had sclerotherapy –
- Teaching should focus on activity restrictions.
- Patients should learn to avoid heavy lifting.
- Teach patients to wait 24 to 48 hours after procedure before showering or taking baths.
- Teach patients to wear supportive stockings as ordered.
- Prepare patients by advising them to expect
ecchymosis and some scarring, which will fade in several weeks. - Caution the patient that some residual brown staining may remain at the injection sites.
- Inform patients that the sclerotherapy may need to be repeated in other areas.
Documentation guidelines
- Physicalassessment of both extremities: Presence of edema, pain, discoloration
- Reaction to the medications used for sclerotherapy and pain management
- Tolerance to activity and exercise
Discharge and home healthcare guidelines
PREVENTION
To prevent worsening of varicosities, health provider are expected to educate patients on how to –
- Avoid prolonged standing in one spot.
- Avoid sitting with legs crossed.
- Elevate the leg(s) frequently during the day.
- Wear support stockings as ordered.
- Lay down on determine posture by orthopedics/physical therapist.
- Drink 1 to 2 Liters of fluid daily.
- Wear shoes that fit comfortably to allow of regular blood flow.
Patients diagnose with varicosities should continue seeing their doctors, nutritionist or health practitioner every 3 months making sure their medical/pathophysiological/wellness conditions demonstrate healthy lifestyle and what is expected to maintain healthy veins.
MEDICATIONS
Teach the patient the purpose, dosage, route, and side effects of any medications ordered.
COMPLICATIONS
Teach the patient to recognize and observe daily for signs of thrombophlebitis, which include redness, local swelling, warmth, discoloration (not related to surgery area), and back pain on bending. Teach the patient which signs to report to the physician.
POSTOPERATIVE COMPLICATIONS
Teach the patient to report any signs of infection, such as redness at incision sites or injection sites, severe pain, purulent drainage, fever, or swelling.